New Computational Model of HIV-HPV Co-infection Predicts Precision Medicine Treatments
In the absence of an effective vaccine, human immunodeficiency virus (HIV), a retrovirus that can cause acquired immunodeficiency syndrome (AIDS), continues to be a major global public health burden. About 36.7 million people worldwide and 1.2 million people in the United States are infected with HIV. No effective cure for HIV exists. Currently, the disease management involves lifelong treatment with combined antiretroviral therapy (cART), which is challenging due to patient compliance issues, drug treatment side effects, and drug resistance.
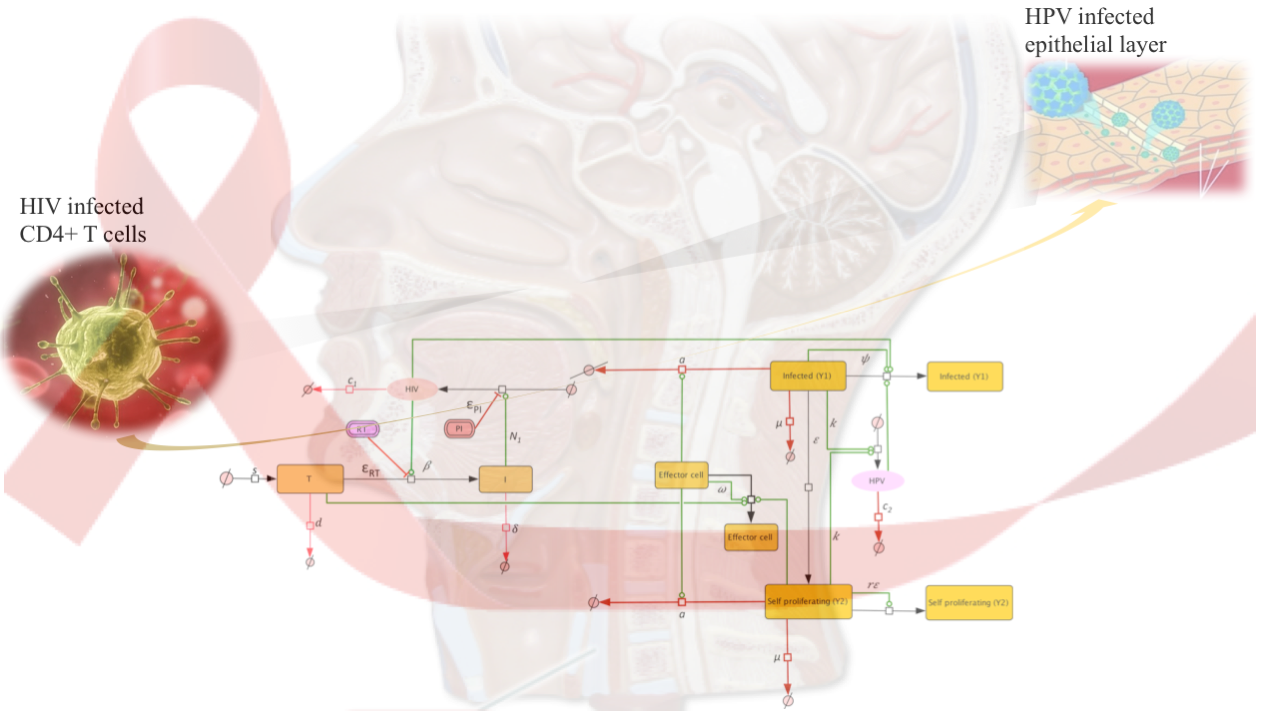
HIV infects CD4+ T cells, which orchestrate immune responses to infections. A decrease in the CD4+ T cell counts due to HIV renders a patient vulnerable to other opportunistic infections and infection-related cancers. In particular, co-infection with human papillomavirus (HPV) leads to increased incidence of oropharyngeal cancers, compared to HPV infections alone.
The Nutritional Immunology and Molecular Medicine Laboratory (NIMML) at the Biocomplexity Institute recently developed a computational model that describes the mechanistic interactions between the HIV and HPV viruses in HIV-HPV co-infected patients. The co-infection model, first of its kind, provided evidence for increased HPV disease due to HIV induced immunosuppression and predicted correlations between the CD4+ T cell restoration during cART therapy and the transition between persistent and resolved HPV infections. The findings were published in a recent paper in PLOS ONE.
“The work highlights the power of mathematical models to study co-infections,” said Meghna Verma, a researcher at Nutritional Immunology and Molecular Medicine Laboratory (NIMML) and graduate student in the Translational Biology Medicine and Health program. “The limited clinical information about treatment and prevention options against HPV in HIV-infected individuals led us to employ modeling approaches to investigate the co-infection. We can use the model simulations to determine how HIV directed therapeutics such as cART can help halt the HPV-related oropharyngeal disease in co-infected individuals.“
The modeling prediction highlights the importance of the timing of cART compared to the timing of HPV co-infection in determining the timing of HPV resolution.
“To study the gut immunity, we have applied transformative modeling technologies driven by high performance computing that improve efficiency, decrease cost and reduce the time required to find treatments for debilitating and widespread diseases such as inflammatory bowel disease (IBD), Helicobacter pylori infection, Clostridium difficile infection. We have built computational and mathematical models of unprecedented scalability (trillions of interactions) and resolution (from molecules to cells, to tissues to systems). Like our previous modeling work, simulation using the new model becomes a better-informed path to precision medicine interventions during co-infection with HIV and HPV,” said Dr. Bassaganya-Riera, Professor of Immunology and Director of the NIMML at Virginia Tech. “Modeling takes us one step closer to next generation precision medicine, encompassing smarter, faster and more accurate decisions. The work is the result of a team science effort between NIMML and Dr. Stanca Ciupe, an Associate Professor at the Department of Mathematics.”
‘’Mathematical models have been an essential tool in assessing the effectiveness of cART in HIV infections. A natural extension is determining the effectiveness of cART therapy in HIV-HPV co-infected individuals. In this study, we investigated how cART can help not just reduce HIV levels but also speed the time of HPV resolution. The computational modeling results were unforeseen. It is known that cART does not interfere with HPV replication. Nevertheless, by restoring the CD4+ T cell mediated immune response, it indirectly strengthens the immune response against HPV’’, said Dr. Stanca Ciupe, Associate Professor of Mathematics at Virginia Tech. ‘’We found that the HPV oncogenic expression and the timing of cART in relation to the timing of HPV co-infection are important metrics for predicting the time of HPV removal. These results are useful in providing guidance for personalized treatments in co-infected patients”.
The work was awarded as listed as the top awardee at the Research Symposium, 2016 poster session held at the Biocomplexity Institute of Virginia Tech on November 1, 2016. For more information and access to the symposium videos and panel discussion, please visit here.
The new mechanistic model of HIV/HPV co-infection has been deposited at biomodels.net and it can be downloaded here.
Related Press releases:
Learning computational immunology
About NIMML
The NIMML Institute is a 501 (c) (3) non-profit public charity foundation focused on a transdisciplinary, team-science approach to precision medicine at the interface of immunology, inflammation, and metabolism. The NIMML Institute team has led numerous large-scale transdisciplinary projects and is dedicated to solving important societal problems by combining the expertise of immunologists, computational biologists, toxicologists, modelers, translational researchers, and molecular biologists. The Institute is headquartered in Blacksburg, VA. For more information, please visit www.nimml.org or contact pio@nimml.org.